Blood pressure above 180/120 mmHg can trigger severe headaches that differ significantly from typical tension headaches or migraines. These hypertensive headaches occur when extremely high blood pressure causes increased pressure within blood vessels in the brain, leading to distinctive symptoms that require immediate medical attention.
Hypertension headaches develop through a specific mechanism: when blood pressure reaches dangerously high levels, the blood-brain barrier becomes compromised, allowing fluid to leak into surrounding brain tissue. This creates pressure and swelling that manifests as intense head pain, often accompanied by neurological symptoms.
Recognizing Hypertension Headache Symptoms
Hypertensive headaches present with specific characteristics that distinguish them from other headache types. The pain typically develops as a pulsating sensation on both sides of the head, intensifying with physical activity or sudden movements. Unlike migraines that may affect one side, hypertensive headaches create symmetrical pressure that patients often describe as feeling like their head might explode.
Visual disturbances accompany many hypertensive headaches. Patients report blurred vision, seeing spots or flashing lights, and temporary blind spots in their visual field. These symptoms result from increased pressure affecting the optic nerves and blood vessels supplying the eyes. Double vision may occur when blood pressure severely impacts the muscles controlling eye movement.
Morning headaches that improve throughout the day often indicate nocturnal blood pressure spikes. Blood pressure naturally rises in early morning hours, and individuals with uncontrolled hypertension may experience their highest readings during sleep. These headaches typically present as dull, persistent pain upon waking that gradually subsides as blood pressure normalizes with daily activity.
Accompanying symptoms provide important diagnostic clues. Nosebleeds occur when fragile nasal blood vessels rupture under extreme pressure. Facial flushing results from dilated blood vessels near the skin surface. Some patients experience pulsatile tinnitus—hearing their heartbeat in their ears—due to increased blood flow through temporal arteries. Nausea and vomiting may develop when increased intracranial pressure affects the brain’s vomiting center.
Blood Pressure Levels and Headache Risk
Hypertensive urgency occurs when blood pressure exceeds 180/120 mmHg without immediate organ damage. During these episodes, headaches develop as the body’s warning signal that blood pressure has reached dangerous levels. The brain’s autoregulation mechanisms, which normally maintain stable blood flow despite pressure changes, become overwhelmed at these extreme readings.
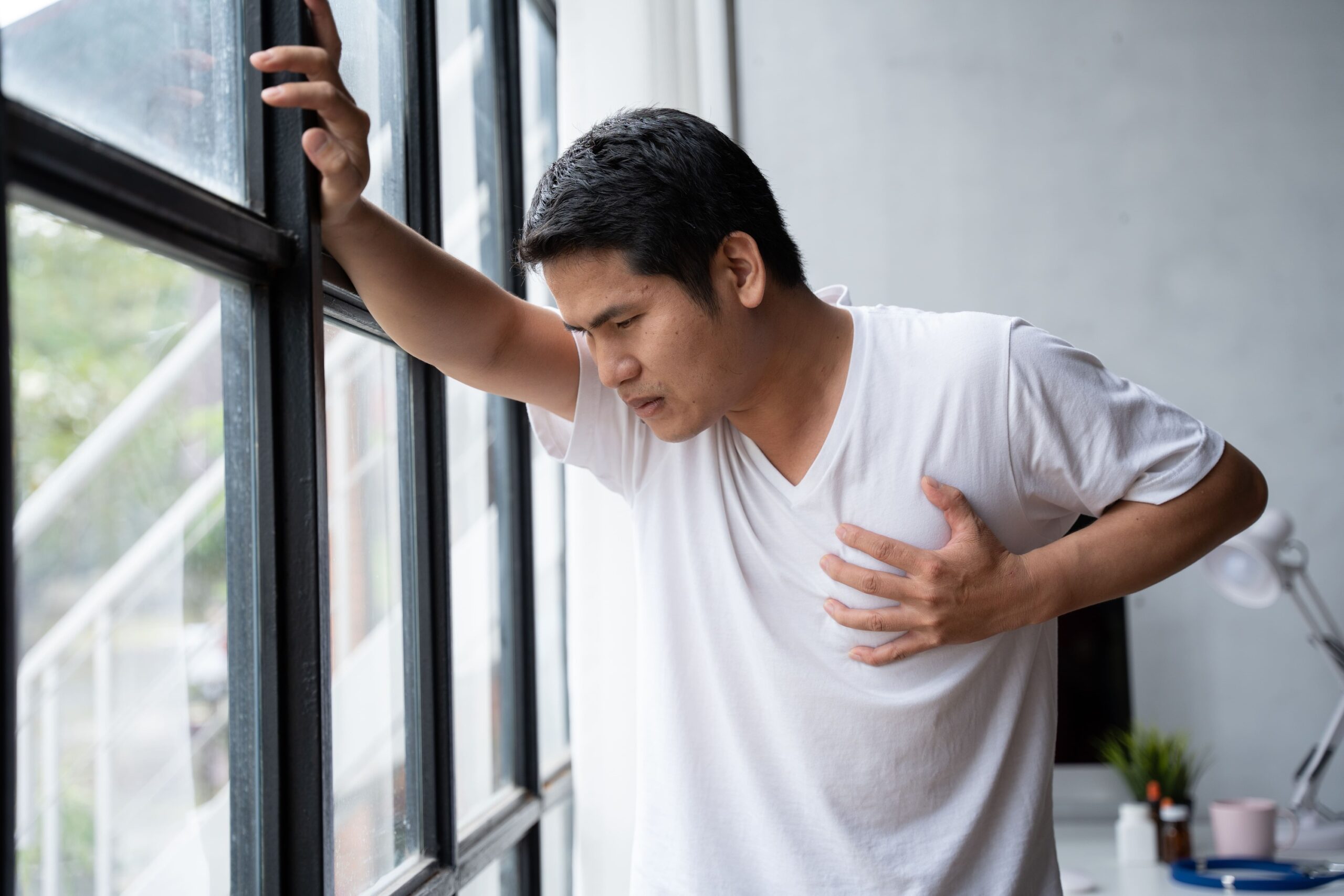
Hypertensive emergency represents a more severe condition where blood pressure above 180/120 mmHg causes active organ damage. Headaches during hypertensive emergencies often accompany chest pain, shortness of breath, numbness, or difficulty speaking. These symptoms indicate potential damage to the heart, kidneys, brain, or blood vessels requiring immediate emergency department evaluation.
Blood pressure variability plays an important role in headache development. Rapid fluctuations in blood pressure, even within the high-normal range, can trigger headaches in sensitive individuals. Patients who experience blood pressure swings of 20-30 mmHg within short periods report more frequent headaches than those with stable readings.
Secondary hypertension from underlying conditions produces distinctive headache patterns. Pheochromocytoma, a rare adrenal gland tumor, causes sudden severe headaches with profuse sweating and rapid heartbeat. Kidney disease-related hypertension often produces persistent dull headaches that worsen with fluid retention. Recognizing these patterns helps identify treatable causes of both high blood pressure and associated headaches.
Immediate Management Strategies
During a suspected hypertensive headache, proper positioning can provide relief while awaiting medical evaluation. Sitting upright with the head elevated at 30-45 degrees reduces intracranial pressure and promotes venous drainage from the brain. Lying flat often worsens symptoms by increasing blood flow to the head. Support the neck and shoulders to minimize muscle tension that could exacerbate pain.
Creating a calm environment helps lower blood pressure naturally. Dim lighting reduces sensory stimulation that can intensify both headaches and blood pressure. Cool temperatures promote vasoconstriction and may provide symptomatic relief. Remove tight clothing, especially around the neck, to improve circulation and reduce perceived pressure.
Breathing techniques offer immediate blood pressure reduction. The 4-7-8 breathing pattern—inhaling for 4 counts, holding for 7, exhaling for 8—activates the parasympathetic nervous system and lowers blood pressure within minutes. Deep diaphragmatic breathing increases oxygen delivery while reducing stress hormones that elevate blood pressure.
💡 Did You Know?
The brain has specialized cells called baroreceptors that detect blood pressure changes and trigger protective responses. During hypertensive episodes, these cells become overwhelmed, contributing to headache development through altered nerve signaling.
Hydration status significantly impacts both blood pressure and headache severity. Dehydration concentrates blood sodium levels, increasing blood pressure and headache risk. Drinking room temperature water slowly helps restore blood volume without causing rapid fluid shifts. Avoid ice-cold beverages that can trigger reflex blood vessel constriction.
Long-Term Prevention and Management
Medication adherence forms the foundation of hypertensive headache prevention. ACE inhibitors and ARBs not only lower blood pressure but also protect blood vessels from damage that contributes to headaches. Beta-blockers reduce both blood pressure and headache frequency by decreasing stress hormone effects. Calcium channel blockers prevent blood vessel spasm that can trigger both hypertension and headaches.
Dietary modifications target multiple mechanisms of blood pressure control. The DASH eating pattern emphasizes potassium-rich foods that counteract sodium’s effects. Limiting sodium to less than 2,300 mg daily reduces fluid retention and blood vessel stiffness. Magnesium-rich foods like leafy greens and nuts support blood vessel relaxation and may reduce headache frequency.
Regular blood pressure monitoring identifies patterns that predict headache risk. Morning and evening measurements capture daily variations. Recording readings alongside headache occurrences reveals individual trigger points—some patients develop headaches at 160/100 mmHg while others remain symptom-free until 180/110 mmHg. Modern home monitors store readings electronically, creating valuable data for medical consultations.
Sleep quality directly impacts blood pressure control and headache prevention. Sleep apnea causes repeated blood pressure spikes throughout the night, leading to morning headaches and sustained hypertension. Maintaining consistent sleep schedules supports natural blood pressure rhythms. Elevating the head of the bed 15-30 degrees reduces nocturnal blood pressure and morning headache severity.
⚠️ Important Note
Never attempt to rapidly lower blood pressure during a hypertensive headache without medical supervision. Sudden blood pressure drops can cause stroke or heart attack by reducing blood flow to vital organs that have adapted to higher pressures.
What Our Internal Medicine Specialists Say
Internal medicine physicians recognize hypertensive headaches as important warning signals requiring comprehensive evaluation. While treating the immediate headache provides relief, identifying and addressing underlying blood pressure control issues prevents future episodes and potential organ damage.
Specialist evaluation includes 24-hour ambulatory blood pressure monitoring to capture patterns missed during office visits. This reveals nocturnal hypertension, white coat syndrome, and masked hypertension—conditions that significantly impact headache risk but remain hidden during routine checks. Specialists also investigate secondary causes through targeted testing based on symptom patterns and physical examination findings.
Treatment approaches extend beyond blood pressure medications. Specialists may recommend specific headache preventive medications for patients with frequent hypertensive headaches. Lifestyle interventions receive equal emphasis, with structured programs addressing weight management, stress reduction, and exercise prescription tailored to individual cardiovascular risk profiles.
Putting This Into Practice
- Track blood pressure readings twice daily at consistent times, recording any associated headache symptoms, their severity, and duration in a dedicated log or smartphone app
- Create a headache action plan listing specific blood pressure thresholds that trigger different responses—home management techniques for readings below 160/100 mmHg versus immediate medical contact for readings above 180/120 mmHg
- Establish a morning routine that includes gentle stretching, controlled breathing exercises, and gradual position changes to prevent rapid blood pressure fluctuations that trigger headaches
- Modify your workspace ergonomics to maintain proper neck alignment and reduce muscle tension that compounds hypertensive headaches—position monitors at eye level and use supportive seating
- Develop meal prep strategies focusing on low-sodium, high-potassium options that support blood pressure control while maintaining variety and palatability in your daily diet
When to Seek Professional Help
- Sudden severe headache with blood pressure above 180/120 mmHg
- Headache accompanied by chest pain, shortness of breath, or irregular heartbeat
- Vision changes including blurred vision, double vision, or temporary blindness
- Confusion, difficulty speaking, or understanding speech during headache episodes
- Weakness or numbness in face, arms, or legs alongside headache
- Persistent headaches despite taking prescribed blood pressure medications
- Morning headaches occurring more than twice weekly
- Headaches with severe nausea and repeated vomiting
- Nosebleeds occurring simultaneously with severe headaches
Commonly Asked Questions
Can normal blood pressure readings still cause headaches?
Blood pressure fluctuations within the normal range rarely cause true hypertensive headaches. However, rapid changes from low-normal to high-normal readings may trigger headaches in sensitive individuals. Stress, dehydration, and certain medications can cause these fluctuations even when average readings remain normal.
How quickly do hypertensive headaches resolve after blood pressure treatment?
Hypertensive headaches typically improve within 1-2 hours of achieving blood pressure reduction below 160/100 mmHg. Complete resolution may take 4-6 hours as brain swelling subsides. Headaches persisting beyond 24 hours despite normalized blood pressure require further evaluation for other causes.
Should I take pain medication for hypertensive headaches?
Acetaminophen provides safer pain relief than NSAIDs during hypertensive episodes, as NSAIDs can increase blood pressure and reduce kidney function. However, addressing the underlying blood pressure elevation remains the primary treatment. Never use pain medication as a substitute for blood pressure management.
Can hypertensive headaches occur without other symptoms?
Isolated headaches rarely represent true hypertensive headaches. Most patients experience additional symptoms like visual changes, dizziness, or palpitations. Headaches occurring alone with mildly elevated blood pressure more likely represent tension headaches or migraines coinciding with stress-induced blood pressure rises.
Do all people with high blood pressure get headaches?
Many individuals with chronic hypertension never experience headaches, as their bodies adapt to sustained pressure elevations. Headaches typically occur with acute severe elevations or rapid blood pressure changes rather than stable chronic hypertension.
Next Steps
Hypertensive headaches signal dangerous blood pressure elevations requiring immediate attention and ongoing management. Recognizing their distinctive features—bilateral pulsating pain with visual disturbances and morning predominance—enables timely intervention. Combining acute management strategies with long-term blood pressure control prevents both headache recurrence and serious cardiovascular complications.
If you’re experiencing recurring headaches with elevated blood pressure readings, our MOH-accredited internal medicine and hypertension specialists can provide comprehensive evaluation and personalized treatment strategies.