Blood pressure readings above 140/90 mmHg on multiple occasions indicate hypertension, requiring careful evaluation for treatment. Singapore’s clinical guidelines recommend medication therapy based on specific thresholds, cardiovascular risk factors, and individual patient characteristics. The decision to start hypertension medications involves more than just blood pressure numbers—it encompasses overall cardiovascular risk assessment, lifestyle factors, and potential medication benefits versus risks.
Treatment approaches vary significantly between patients with Stage 1 hypertension (140-159/90-99 mmHg) and those with Stage 2 hypertension (≥160/100 mmHg). While Stage 2 hypertension typically requires immediate medication therapy, Stage 1 cases may warrant a trial of lifestyle modifications first, particularly in younger patients without additional risk factors.
Blood Pressure Thresholds for Treatment
Clinical guidelines establish clear blood pressure thresholds for initiating medication therapy. Patients with blood pressure readings consistently ≥160/100 mmHg require immediate medication treatment, regardless of other factors. This Stage 2 hypertension poses significant cardiovascular risks that lifestyle modifications alone cannot adequately address.
For Stage 1 hypertension (140-159/90-99 mmHg), treatment decisions become more nuanced. Patients with diabetes, chronic kidney disease, or established cardiovascular disease should start medications immediately, even at these lower thresholds. The presence of target organ damage—such as left ventricular hypertrophy, proteinuria, or retinopathy—also necessitates prompt medication therapy.
Younger patients under 40 with Stage 1 hypertension and no additional risk factors may trial lifestyle modifications for 3-6 months before starting medications. During this period, regular blood pressure monitoring every 4-6 weeks tracks response to lifestyle changes. If blood pressure remains elevated after this trial period, medication therapy becomes necessary.
The concept of cardiovascular risk stratification guides treatment timing. Patients with a 10-year cardiovascular risk exceeding 20% benefit from immediate medication therapy, even with Stage 1 hypertension. Risk calculators incorporate factors like age, cholesterol levels, smoking status, and diabetes to generate these estimates.
First-Line Medication Classes
Four medication classes serve as first-line options for hypertension treatment, each with distinct mechanisms and patient-specific advantages. ACE inhibitors (like enalapril or perindopril) work by blocking the renin-angiotensin system, reducing blood vessel constriction and lowering blood pressure. These medications particularly benefit patients with diabetes or chronic kidney disease, as they provide additional kidney protection beyond blood pressure control.
Angiotensin receptor blockers (ARBs) such as losartan or telmisartan offer similar benefits to ACE inhibitors through a slightly different mechanism. ARBs become the preferred choice for patients who develop a persistent dry cough with ACE inhibitors—a side effect occurring in some users. Both ACE inhibitors and ARBs require periodic monitoring of kidney function and potassium levels.
Calcium channel blockers like amlodipine or nifedipine relax blood vessel walls directly, making them particularly effective in older patients. These medications rarely cause metabolic disturbances, making them suitable for patients with diabetes or metabolic syndrome. The dihydropyridine class (amlodipine, nifedipine) may cause ankle swelling in some patients, while non-dihydropyridines (diltiazem, verapamil) can slow heart rate.
Thiazide-like diuretics such as chlorthalidone or indapamide reduce blood volume through increased urine production. These medications demonstrate particular effectiveness in preventing stroke and work well in combination with other antihypertensives. Low doses minimize metabolic effects while maintaining blood pressure benefits. Regular monitoring of electrolytes, particularly potassium and sodium, ensures safe long-term use.
Combination Therapy Approaches
Most patients with hypertension require multiple medications to achieve target blood pressure levels. Starting with combination therapy proves more effective than sequential monotherapy for patients with blood pressure >20/10 mmHg above target or those with Stage 2 hypertension. Fixed-dose combinations improve medication adherence by reducing pill burden.
Effective combinations pair medications with complementary mechanisms. ACE inhibitors or ARBs combine well with calcium channel blockers or diuretics. This approach targets both vasoconstriction and volume regulation simultaneously. Combining an ACE inhibitor with an ARB provides no additional benefit and increases adverse effect risks, making this combination inappropriate.
💡 Did You Know?
Fixed-dose combination pills containing two or three medications in one tablet improve blood pressure control through enhanced adherence. Patients taking single-pill combinations demonstrate better long-term blood pressure control compared to those taking the same medications separately.
Triple therapy becomes necessary when dual combinations fail to achieve target blood pressure. The standard approach combines an ACE inhibitor or ARB with a calcium channel blocker and a diuretic. This combination addresses multiple pathways contributing to hypertension while maintaining tolerability.
Resistant hypertension—blood pressure remaining above target despite three medications at optimal doses, including a diuretic—requires specialist evaluation. Adding spironolactone as a fourth agent often proves effective, particularly in patients with underlying aldosterone excess. Alternative fourth-line options include beta-blockers, alpha-blockers, or centrally acting agents, chosen based on individual patient characteristics.
Special Populations and Medication Selection
Pregnant women with hypertension require specific medication choices to ensure fetal safety. Methyldopa, labetalol, and nifedipine remain the preferred options during pregnancy. ACE inhibitors and ARBs cause fetal abnormalities and must be discontinued before conception or immediately upon pregnancy confirmation. Women of childbearing age taking these medications need reliable contraception and preconception counseling.
Patients with chronic kidney disease benefit from ACE inhibitors or ARBs, which slow kidney disease progression beyond their blood pressure effects. These medications reduce proteinuria and preserve kidney function, particularly in diabetic kidney disease. Serum creatinine may increase up to 30% after initiation—this expected change doesn’t require discontinuation unless it exceeds this threshold or hyperkalemia develops.
Diabetic patients often require multiple medications to achieve the recommended target of <130/80 mmHg. ACE inhibitors or ARBs provide first-line therapy due to their kidney-protective effects. Adding calcium channel blockers or diuretics as second-line agents helps achieve targets while minimizing metabolic disturbances. Beta-blockers may mask hypoglycemia symptoms and worsen glucose control, limiting their use in diabetes.
⚠️ Important Note
Elderly patients require careful medication titration due to increased sensitivity and fall risk. Starting doses should be half the standard adult dose, with gradual increases every 2-4 weeks while monitoring for orthostatic hypotension and adverse effects.
Patients with previous stroke benefit from blood pressure reduction regardless of baseline levels. Combination therapy with an ACE inhibitor plus diuretic or calcium channel blocker demonstrates improved stroke prevention compared to monotherapy. Target blood pressure for secondary stroke prevention remains <130/80 mmHg.
Monitoring and Adjusting Treatment
Initial medication response requires assessment within 4-6 weeks of starting therapy. Blood pressure measurements should occur at similar times of day, after 5 minutes of seated rest, using proper technique. Home blood pressure monitoring provides valuable data between clinic visits, with readings <135/85 mmHg indicating good control.
Laboratory monitoring ensures medication safety and efficacy. Baseline tests include serum creatinine, electrolytes, and liver function. ACE inhibitors and ARBs require repeat testing 1-2 weeks after initiation and dose increases, then every 6-12 months once stable. Diuretics need periodic electrolyte monitoring, particularly in elderly patients or those on multiple medications affecting potassium.
✅ Quick Tip
Keep a blood pressure diary recording morning and evening readings for one week before each clinic visit. This provides your physician with valuable data for optimizing medication timing and dosing.
Medication side effects requiring dose adjustment or drug changes occur frequently during initial treatment. Switching within medication classes (such as from one ACE inhibitor to another) may resolve side effects while maintaining efficacy. Timing adjustments—such as taking diuretics in the morning to avoid nighttime urination—improve tolerability without changing medications.
Target blood pressure achievement typically requires 3-6 months of systematic adjustments. Once target blood pressure is achieved and maintained for 6-12 months, some patients may qualify for careful dose reduction under medical supervision.
What Our Internal Medicine Specialist Says
Successful hypertension management extends beyond simply prescribing medications. Patients benefit most when they understand their target blood pressure, monitor regularly at home, and communicate openly about side effects or concerns. Many patients fear lifelong medication dependency, but achieving good blood pressure control often allows for dose reductions or simplified regimens over time.
The choice between starting one medication versus combination therapy depends on multiple factors beyond just blood pressure numbers. Patients with blood pressure 150/95 mmHg might start with monotherapy if they’re young with no other risk factors, while someone with the same reading but diabetes would benefit from initial combination therapy. This individualized approach maximizes effectiveness while minimizing side effects.
Medication timing significantly impacts both efficacy and tolerability. Taking long-acting medications at bedtime may provide better 24-hour control and reduce morning blood pressure surge. However, diuretics should be taken in the morning to avoid sleep disruption. These practical considerations often determine treatment success as much as medication selection itself.
Putting This Into Practice
- Request home blood pressure monitoring education from your healthcare provider, including proper cuff size selection and measurement technique for accurate readings
- Create a medication schedule that aligns with your daily routine, setting phone reminders for consistent timing and tracking any symptoms or side effects in a diary
- Prepare a list of all current medications, supplements, and over-the-counter drugs for each medical appointment, as many can interact with blood pressure medications
- Schedule laboratory tests as recommended by your physician, typically every 3-6 months initially, then annually once stable on therapy
- Develop a plan with your physician for managing blood pressure during illness, travel, or other disruptions to routine that might affect medication adherence
When to Seek Professional Help
- Blood pressure readings consistently above 180/110 mmHg
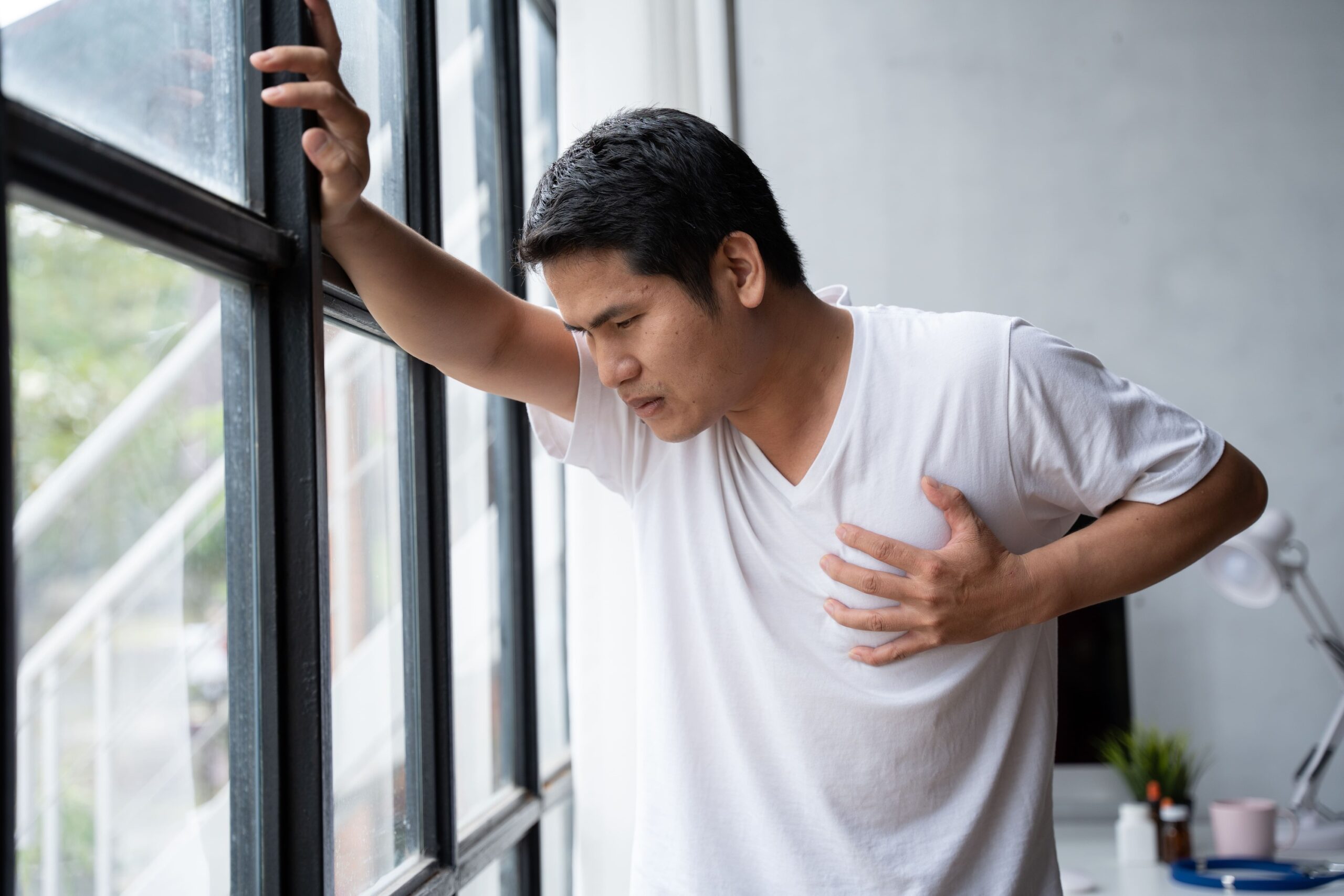
- Chest pain, severe headache, or vision changes with elevated blood pressure
- Dizziness, frequent falls, or fainting after starting new medications
- Persistent dry cough, ankle swelling, or other bothersome side effects
- Blood pressure remaining above target after 3 months of treatment
- Difficulty affording prescribed medications
- Planning pregnancy while taking blood pressure medications
- Unexplained fatigue, weakness, or exercise intolerance after medication changes
Commonly Asked Questions
Can I stop medications once my blood pressure normalizes?
Blood pressure medications control rather than cure hypertension. Stopping medications typically causes blood pressure to rise within days to weeks. Some patients achieving good control through weight loss and lifestyle changes may qualify for carefully supervised medication reduction, but complete discontinuation rarely succeeds long-term. Never stop medications without physician guidance.
Why do I need multiple medications when one partially lowers my blood pressure?
Hypertension results from multiple physiological mechanisms—blood vessel stiffness, excess fluid retention, hormonal imbalances, and nervous system activation. Single medications target only one mechanism, achieving limited reduction. Combining medications with different mechanisms provides synergistic effects, achieving better control with lower individual doses and fewer side effects than maximizing single medications.
How long before blood pressure medications show full effect?
Most blood pressure medications require 2-4 weeks to demonstrate full efficacy. ACE inhibitors and ARBs may take 6-8 weeks for maximum effect. Initial blood pressure reduction occurs within days, but blood vessel remodeling and hormonal adjustments continue for weeks. This delayed response explains why medication adjustments should occur at 4-6 week intervals rather than more frequently.
Should I take medications even if I feel fine?
Hypertension remains asymptomatic until organ damage occurs. Medications prevent future complications—stroke, heart attack, kidney failure, and vision loss—rather than treating current symptoms. Consistent medication adherence, regardless of how you feel, provides protection against these complications.
Next Steps
Successfully managing hypertension requires finding the right medication combination for your individual needs. Regular monitoring and open communication with your physician ensure optimal treatment outcomes while minimizing side effects.
If you’re experiencing elevated blood pressure readings or struggling with current hypertension medications, our MOH-accredited internal medicine specialists provide comprehensive evaluation and personalized treatment plans.