Hypertensive urgency occurs when blood pressure suddenly spikes above 180/120 mmHg without immediate organ damage. This condition differs from hypertensive emergency, where the same blood pressure levels cause active organ damage requiring hospitalization. Managing hypertension attack situations requires recognizing specific symptoms and taking measured actions while seeking appropriate medical care.
Blood pressure readings consist of systolic pressure (top number) measuring arterial pressure during heartbeats and diastolic pressure (bottom number) measuring pressure between beats. Normal readings fall below 120/80 mmHg, while readings consistently above 140/90 mmHg indicate hypertension. Sudden elevations beyond 180/120 mmHg demand immediate attention and specific management strategies.
Identifying Hypertensive Urgency Symptoms
Severe headaches localized to the back of the head often signal dangerous blood pressure elevations. These headaches feel different from typical tension headaches, presenting as throbbing pain that worsens with movement or straining. The pain may radiate to the temples and neck, accompanied by sensitivity to light and sound.
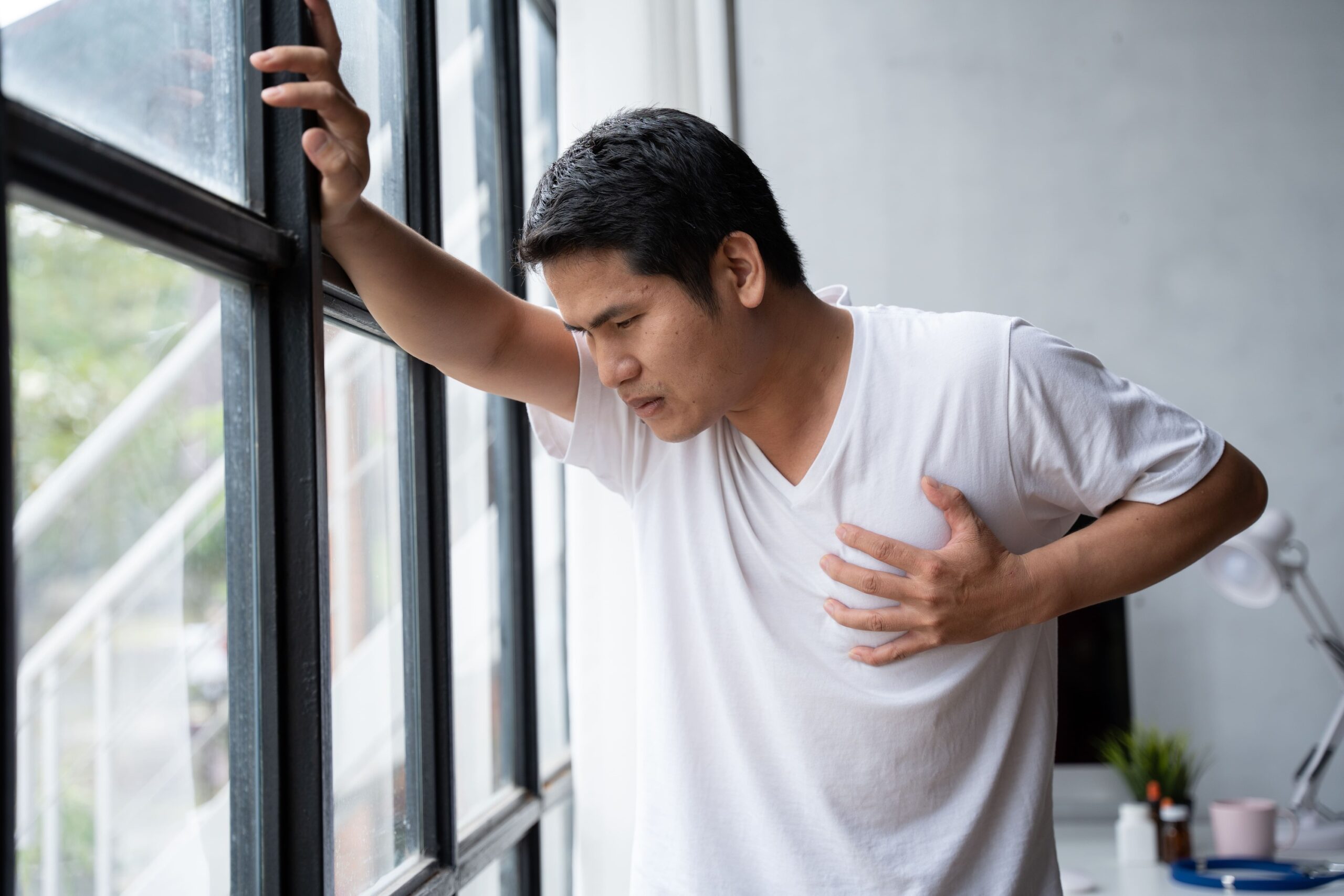
Chest discomfort during hypertensive urgency manifests as pressure or tightness rather than sharp pain. This sensation may spread to the jaw, shoulders, or arms. Some patients describe feeling like an elephant sitting on their chest. This symptom requires immediate blood pressure measurement and medical evaluation to rule out cardiac complications.
Visual disturbances include blurred vision, seeing spots or flashing lights, and temporary vision loss in one or both eyes. These symptoms result from increased pressure affecting the small blood vessels in the retina. Double vision or sudden changes in visual clarity during known hypertension warrant immediate medical attention.
Shortness of breath occurs when elevated blood pressure forces the heart to work harder, potentially causing fluid backup in the lungs. Patients may experience difficulty breathing while lying flat, requiring multiple pillows to sleep comfortably. Sudden onset breathlessness with blood pressure elevation distinguishes this from chronic respiratory conditions.
💡 Did You Know?
The body’s baroreceptors (pressure sensors) can become desensitized to chronically elevated blood pressure, which explains why some patients feel no symptoms even at dangerously high readings. This “silent” presentation makes regular monitoring important for diagnosed hypertension patients.
Immediate Actions During Blood Pressure Spikes
Sit in a comfortable chair with back support and feet flat on the floor. Loosen tight clothing, especially around the neck and waist. Rest quietly for 5-10 minutes before taking blood pressure measurements. Anxiety and movement can temporarily elevate readings by 10-20 mmHg.
Measure blood pressure using a validated home monitor with appropriate cuff size. Take three readings, one minute apart, and record all values with time stamps. The cuff should cover 80% of your upper arm circumference. Position your arm at heart level, supported on a table or armrest.
Deep breathing exercises help activate the parasympathetic nervous system, potentially lowering blood pressure by 5-10 mmHg within minutes. Inhale slowly through your nose for 4 counts, hold for 4 counts, then exhale through pursed lips for 6 counts. Continue this pattern for 5-10 minutes while remaining seated.
Contact your healthcare provider immediately if readings remain above 180/120 mmHg after 30 minutes of rest. Provide all recorded measurements and current symptoms. Your doctor may recommend immediate medication adjustments or advise visiting the emergency department based on your medical history and symptom severity.
⚠️ Important Note
Never attempt to rapidly lower blood pressure through excessive medication doses or unproven methods. Sudden blood pressure drops can reduce blood flow to vital organs, potentially causing stroke or heart attack. Controlled reduction under medical supervision remains the safest approach.
Medication Management Strategies
Short-acting medications provide rapid blood pressure reduction during hypertensive urgency. Sublingual (under tongue) medications work within 15-30 minutes, while oral medications typically take 30-60 minutes. Your specialist prescribes specific “rescue” medications based on your medical history and current medication regimen.
Captopril 25mg sublingual dissolves under the tongue, lowering blood pressure within 15-30 minutes. Maximum effect occurs at 60-90 minutes. This ACE inhibitor works by relaxing blood vessels and reducing the heart’s workload. Monitor blood pressure every 30 minutes after administration.
Labetalol combines alpha and beta-blocking effects, reducing both heart rate and blood vessel resistance. Oral doses of 200-400mg lower blood pressure within 30 minutes to 2 hours. This medication particularly suits patients with concurrent rapid heart rate during hypertensive episodes.
Hydralazine 10-25mg orally acts directly on arterial smooth muscle, causing vessel dilation. Effects begin within 20-30 minutes and peak at 2-4 hours. This medication may cause reflex tachycardia (increased heart rate), making it less suitable for patients with coronary artery disease.
Keep a written record of all medications taken during hypertensive urgency, including exact times and doses. This information helps your specialist adjust your regular medication regimen to prevent future episodes. Never share blood pressure medications with others, as individual responses vary significantly.
Environmental and Lifestyle Modifications
Temperature regulation affects blood pressure through blood vessel constriction and dilation. Move to a cool, quiet room during hypertensive episodes. Remove extra layers of clothing and apply cool (not cold) compresses to wrists and neck. Extreme temperatures in either direction can worsen blood pressure spikes.
Dietary sodium restriction becomes particularly important during acute episodes. Avoid high-sodium foods for 24-48 hours following a hypertensive urgency event. Hidden sodium sources include bread, processed meats, canned soups, and restaurant meals. Fresh fruits, vegetables, and unsalted nuts provide potassium, which helps counteract sodium’s effects.
Sleep position influences blood pressure through gravity’s effect on circulation. Elevate your head 30-45 degrees using pillows or an adjustable bed during hypertensive episodes. Left lateral position (lying on left side) may reduce pressure on major blood vessels, improving circulation and potentially lowering readings.
Stress reduction techniques extend beyond breathing exercises. Progressive muscle relaxation involves tensing and releasing muscle groups systematically, reducing overall tension. Start with toes, work upward through legs, abdomen, arms, and face. Each tension phase lasts 5 seconds, followed by 30 seconds of relaxation.
✅ Quick Tip
Create a “hypertension emergency kit” containing your blood pressure monitor, rescue medications, written emergency instructions from your doctor, and a log book. Store this kit in an easily accessible location known to family members.
What Our Internal Medicine and Hypertension Specialist Says
Hypertensive urgency management requires balancing immediate intervention with long-term control strategies. Patients often focus solely on acute episodes while neglecting daily management. Successful treatment combines appropriate medication timing, lifestyle modifications, and regular monitoring to prevent these dangerous spikes.
Home blood pressure logs reveal patterns invisible during clinic visits. Morning surges, post-meal spikes, and stress-related elevations guide medication timing adjustments. Digital monitors with memory functions help track these patterns, but written logs provide context about activities, symptoms, and medication adherence.
Medication adherence remains the single modifiable factor in preventing hypertensive urgency. Missing doses, especially of short-acting medications, can trigger rebound hypertension within 24-48 hours. Combination pills reduce pill burden and improve adherence, while extended-release formulations provide steadier blood pressure control.
The relationship between salt sensitivity and hypertension varies among individuals. Some patients experience 20-30 mmHg reductions through sodium restriction alone, while others show minimal response. Trial periods of strict sodium restriction help identify responsive patients.
Putting This Into Practice
- Program emergency contacts into your phone under “ICE” (In Case of Emergency), including your hypertension specialist, primary doctor, and preferred hospital
- Establish a blood pressure monitoring routine: measure twice daily at consistent times, recording readings in a dedicated logbook with columns for date, time, blood pressure, pulse, and notes about symptoms or activities
- Create meal plans focusing on DASH diet principles: prepare weekly menus emphasizing whole grains, lean proteins, fruits, vegetables, and low-fat dairy while limiting sodium to less than 2,300mg daily
- Develop a medication organization system using weekly pill boxes, smartphone alarms for dose times, and a backup supply of rescue medications stored in multiple locations
- Design a home environment supporting blood pressure control: install grab bars in bathrooms to prevent straining, arrange furniture to avoid sudden position changes, and maintain comfortable room temperatures between 20-22°C
When to Seek Professional Help
- Blood pressure readings persistently above 180/120 mmHg despite rest and prescribed rescue medications
- Chest pain, pressure, or discomfort spreading to jaw, neck, or arms
- Sudden severe headache different from usual headache patterns
- Difficulty speaking, facial drooping, or arm weakness
- Vision changes including loss of vision, double vision, or seeing halos around lights
- Severe shortness of breath or inability to lie flat
- Confusion, difficulty concentrating, or altered mental state
- Severe anxiety or feeling of impending doom accompanying high blood pressure
- Nosebleeds that won’t stop after 10 minutes of direct pressure
- Blood in urine or decreased urine output
Commonly Asked Questions
How quickly should blood pressure drop during a hypertensive urgency?
Safe blood pressure reduction occurs gradually over 24-48 hours. Initial goals target 10-20% reduction within the first hour, then gradual normalization over days. Rapid drops below 140/90 mmHg can compromise organ blood flow, particularly in patients with longstanding hypertension whose bodies have adapted to higher pressures.
Can I take extra doses of my regular blood pressure medication during a spike?
Taking additional doses of long-acting medications won’t provide immediate relief and may cause dangerous delayed effects. Short-acting rescue medications prescribed specifically for acute episodes work within 30-60 minutes. Contact your specialist before adjusting regular medication doses.
What’s the difference between hypertensive urgency and emergency?
Hypertensive urgency involves blood pressure above 180/120 mmHg without active organ damage. Hypertensive emergency includes the same elevated readings plus evidence of organ damage such as heart attack, stroke, kidney failure, or aortic dissection. Emergency cases require immediate hospitalization and intravenous medications.
Should I go to the emergency room for every blood pressure spike?
Emergency department visits become necessary when blood pressure remains above 180/120 mmHg after following your action plan, or when experiencing symptoms suggesting organ damage. Your specialist provides specific parameters based on your medical history. Many hypertensive urgency cases resolve with home management under medical guidance.
How can I prevent future hypertensive urgency episodes?
Consistent medication adherence prevents most episodes. Take medications at scheduled times, maintain regular follow-ups for dosage adjustments, and monitor blood pressure daily. Identify personal triggers through careful logging, address sleep apnea if present, and maintain stable weight and sodium intake.
Next Steps
Managing hypertension attack situations requires preparation, appropriate response protocols, and ongoing medical supervision. Regular monitoring, medication adherence, and lifestyle modifications reduce episode frequency and severity. Partner with your healthcare team to develop personalized action plans addressing your specific risk factors and medical history.